Glatiramer acetate and interferon beta-1a used in combination were no more effective for patients with relapsing-remitting multiple sclerosis than were either agent alone in a 3-year, randomized trial.
On quality of life measures, monotherapy and combination therapy proved largely equal – and equally well tolerated – in the “CombiRx” study, in which half of the patients got the combination and a quarter got either glatiramer acetate (Copaxone) or interferon beta-1a (Avonex) alone plus a placebo.
CombiRx was conceived at time when interferon beta-1a (IFN-beta-1a) and glatiramer acetate (GA) were the only disease-modifying options for MS; investigators naturally wondered if they’d work better together, said Dr. Lael Stone, a CombiRx investigator and MS specialist at the Cleveland Clinic.
But with natalizumab and fingolimod now on the market, and dimethyl fumarate (also known as BG-12) in the Food and Drug Administration pipeline, times have changed.
It’s never been common to use GA and IFN-beta-1a together, and with newer agents available, “we look at [the CombiRx findings] in 2012 and say ‘that’s not very interesting.’ There were slight indications that” the combination, or one agent or the other, was “better in this respect and not so good in that respect, but it was relatively underwhelming,” Dr. Stone said at the Fourth Cooperative Meeting on Multiple Sclerosis.
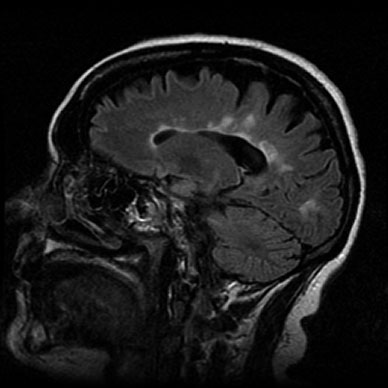
The size of the study – 1,008 treatment-naive patients – and its duration are what remain important. “They can pull out all sorts of other types of data about what happens to MRIs and what happens to the quality of life” in MS. “They can also look at biomarkers [and genetics]. The database was just locked in April, so this is still going to be gone through in much more detail. What’s going to be most interesting are the other things that come out” of this study, she said.
Almost three-quarters of the CombiRx participants were women. They were 38 years old, on average, and 88% of them were white. Their mean baseline Expanded Disability Status Scale (EDSS) score was about 2.0, and mean disease duration 1.2 years.
Almost half the participants reported very good general health at baseline and 37% excellent general health. Most remained healthy throughout the study. “Everyone did very well. There were very minimal changes from baseline to the last observed MSQLI [Multiple Sclerosis Quality of Life Inventory],” the battery of scales used in CombiRx to see how participants fared, said investigator Stacey Cofield, Ph.D., a biostatician at the University of Alabama at Birmingham.
Mental health and perceived-support scores actually improved over the course of the study, she said, although fatigue, bladder, bowel, and cognitive impairment scores worsened slightly. Overall, “these were very small changes. None of them stand out as being very meaningful,” Dr. Cofield said.
Combination therapy showed a half-point benefit on the 22-point bladder control scale, the only scale out of 11 that showed any significant difference between mono and combination therapy.
In the monotherapy groups, IFN-beta-1a patients fared slight better than GA patients on the mental health scale, with no change in the IFN-beta-1a group, but a 3.3 point drop in the 100-point scale in the GA group over 3 years. Conversely, GA patients fared slightly better on the bladder scale, with a 1.5 point improvement vs. a 0.6 point improvement in the IFN-beta-1a group.
Overall, CombiRx had “very low rates of progression and very low amounts of MRI activity,” Dr. Cofield said at the meeting, sponsored by the Consortium of Multiple Sclerosis Centers and the Americas Committee on Treatment and Research in Multiple Sclerosis.
Dr. Cofield reported financial ties to Teva Neuroscience and Centocor Ortho Biotech Services. Other investigators reported numerous ties to pharmaceutical companies, including Teva Neuroscience, which donated the Copaxone used in the trial, and Biogen Idec, which donated the Avonex.